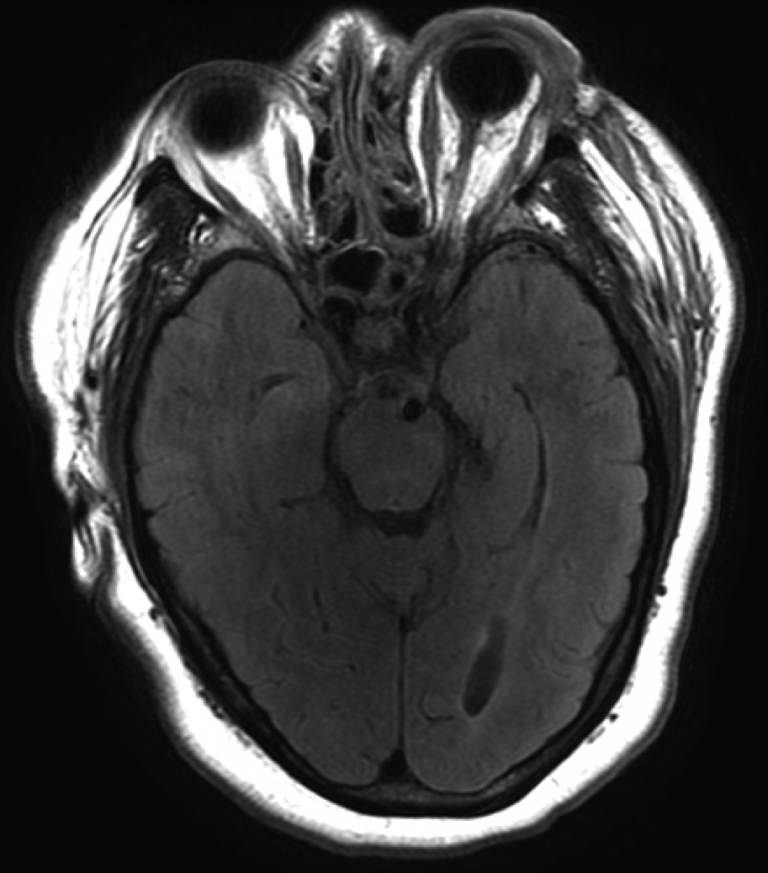
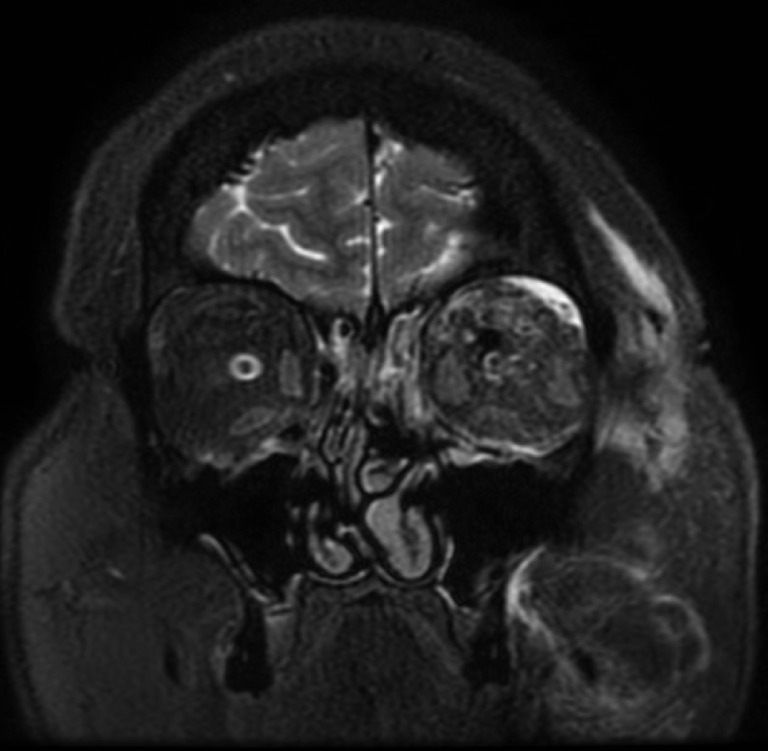
Left internal carotid artery injection, transfacial view demonstrates nearly immediate shunting of arterial blood into the left cavernous sinus. The left sided arterial system flow continues and ACA and MCA filling is superimposed on diffuse venous outflow routes. Venous drainage pathways are bilateral, and there is robust cross-flow from the left cavernous sinus through the intercavernous sinus to the right cavernous sinus. Venous drainage is seen through the petrosal sinuses, pterygoid plexus, and ophthalmic veins.