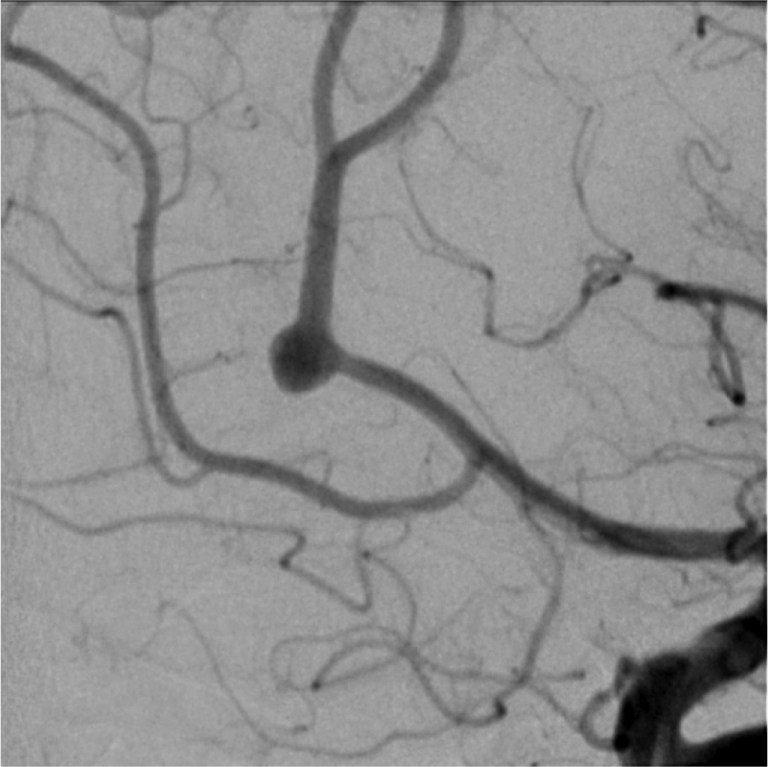
Magnified left ICA injection image, lateral view demonstrates the aneurysm in greater detail.
Left ICA injection, Townes view shows brisk filling of the anterior cerebral artery and middle cerebral artery candelabras. There is a wide necked pericallosal aneurysm that is not associated with a branch artery origin.
Left ICA injection, lateral view shows brisk filling of the anterior cerebral artery and middle cerebral artery candelabras. There is a wide necked pericallosal aneurysm that is not associated with a branch artery origin.